The Brachial Plexus Within the Neck; from Roots to Cords
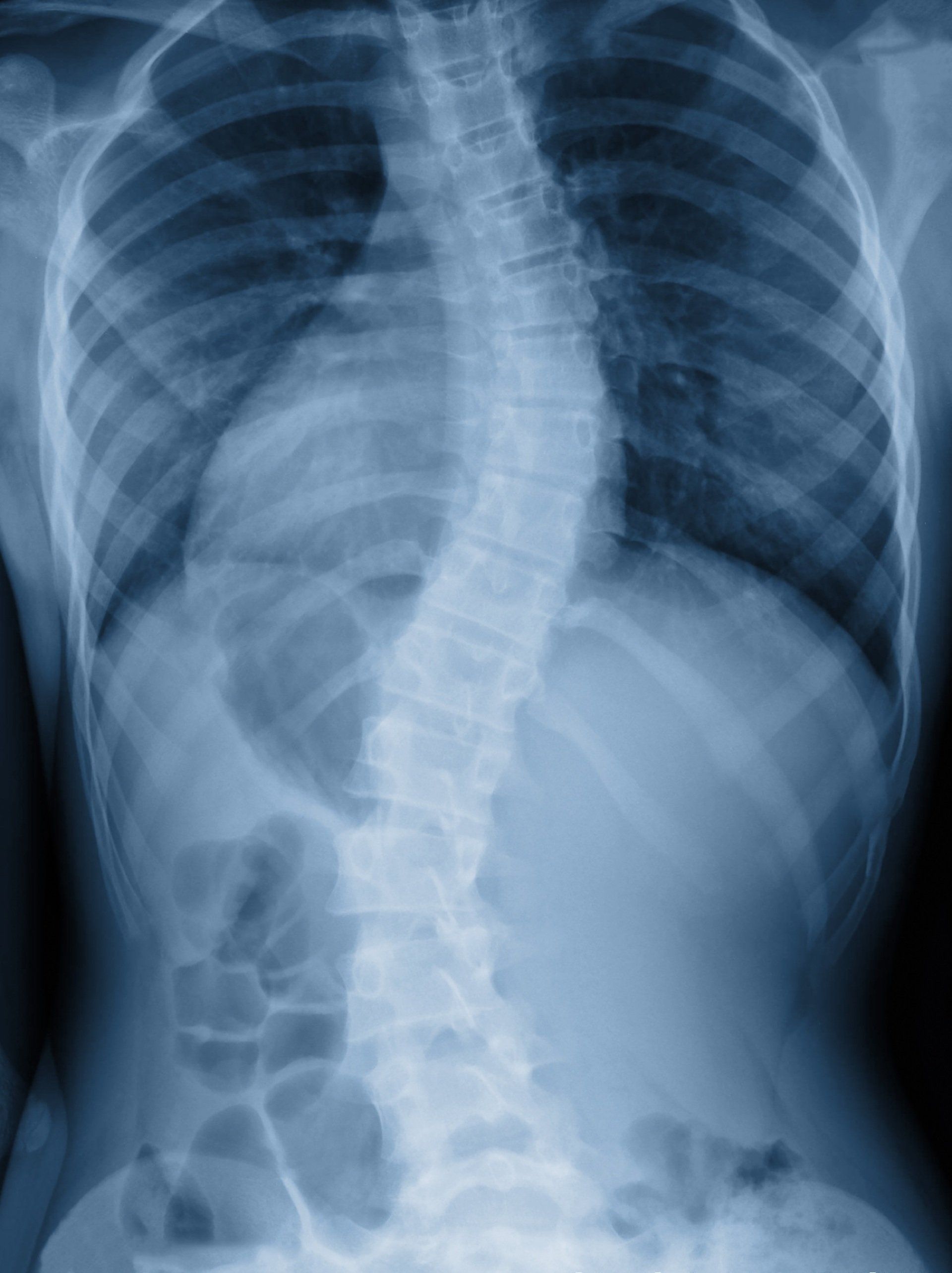
The Brachial Plexus (C5, C6, C7, C8 & T1)
The brachial plexus transmits signals for motor and sensory innervation andsupplies and controls the skin, musculature, sensations and movementsfor the upper extremities including the shoulder, arm, and hands. Without our brachial plexus, we would be unable to perform the various movements which we automatically perform on a daily basis with our upper limbs.
Both 'brachial' and 'plexus' are Latin words, with 'Brachial' stemming from 'brachialis', meaning 'belonging to the arm'. The term 'plexus' means a network (i.e. blood vessels or nerves) or a structure containing a complex network of parts (1).
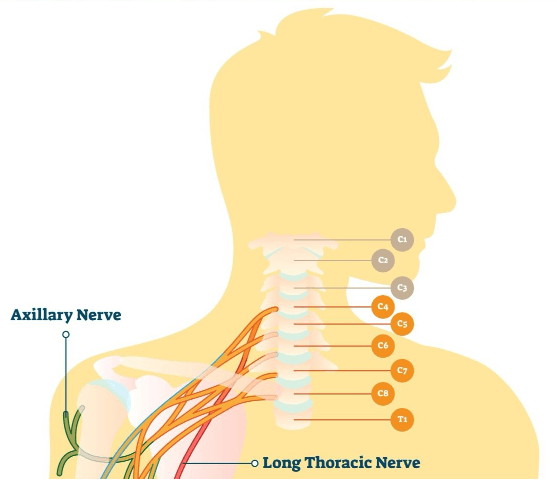
The plexus starts in the neck and is positioned between the neck muscles of the anterior and middle scalenes before passing through the axilla (or armpit) and descending down the arm to supply and innervate muscles, joints and skin of the whole arm and hand (10).
Knowing the brachial plexus and its neural branches is important for practitioners to know, as it can help determine whether a portion of the brachial plexus has been injured which can help tell us which of the associated muscles might be affected before being tested for evidence of a nerve injury (4).
The Brachial Plexus; A Neural Network
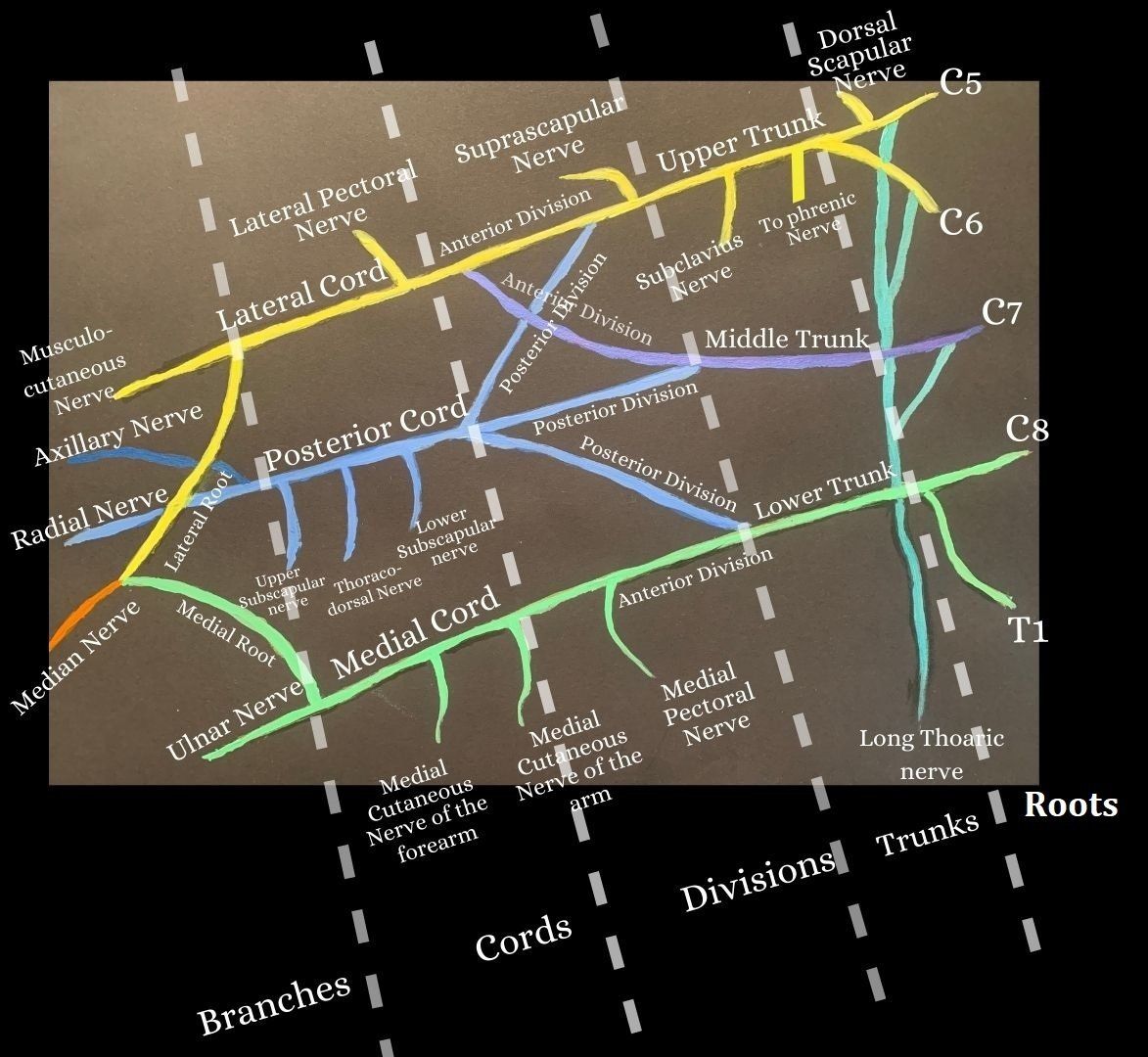
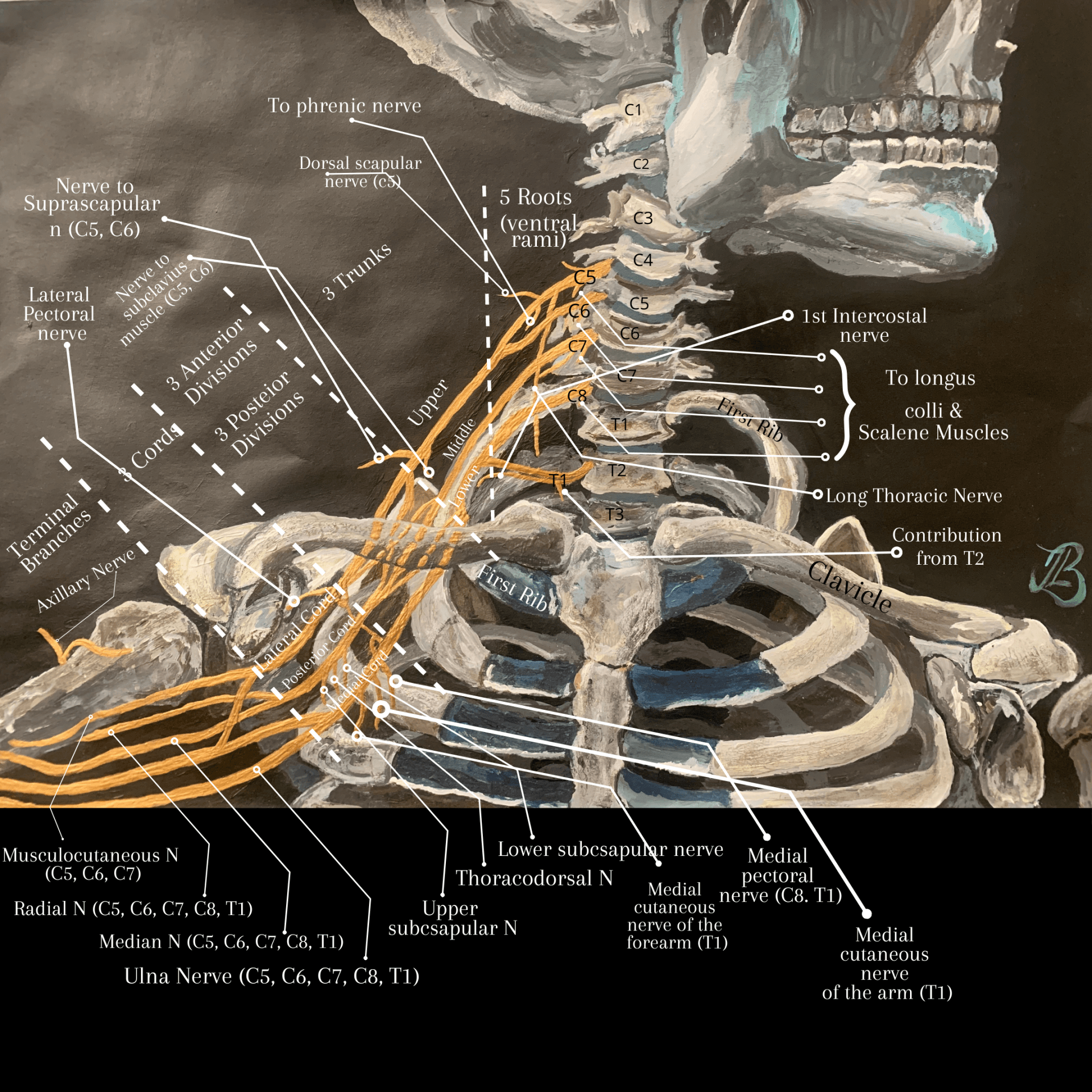
As the nerve roots exit the cervical and thoracicintervertebral foramen, or bony openings found between adjacent vertebrae, they unite and branch in the following order: roots, trunks, divisions, cords, terminal branches
(and peripheral nerves) (10, 3). A helpful mnemonic for this is; R
ead T
hat D
eadly C
adaver B
ook (10). There is no difference in terms of function between each division and they are simply used as an aid to further explain or remember the brachial plexus (10).
The Roots
The first section of the brachial plexus with each spinal level having four nerve roots as there are two spinal nerve roots for the left and right side; the posterior (dorsal) and anterior (ventral) nerve roots. The anterior (ventral) nerve roots carry motor signals from the brain to the muscles and the posterior (dorsal) roots carry sensory signals from the skin to the brain (10). The anterior and posterior roots combine to form a spinal nerve at each intervertebral foramen (9).
The brachial plexus is formed by the anterior rami
of cervical spinal nerves C5, C6, C7 and C8, and the first thoracic spinal nerve, T1. They unite in the neck between the anterior and middle scalene muscles, to form the trunks after the roots. The emergence of each root can be read below and followed from figure 1 and figure 2:
1st root
: arises from the anterior ramus of C5 above
the 5th cervical vertebra (figure 1.).
2nd root:
Arises from the anterior ramus of C6 below
C5.
3rd root:
From the anterior ramus of C7 below
C6.
4th root:
From the anterior ramus of C8 emerges above
the first thoracic vertebra.
5th root:
Arises from the anterior ramus of T1 emerges below
the first thoracic vertebra (3).
The Trunks
The three trunks of the brachial plexus originate from the roots and are located within the lower part of the posterior cervical triangle, they passes laterally over the first rib before entering the axilla (2, 3).
The Superior Trunk: The first of the three trunks is the upper (superior) trunk and is formed by the union of the anterior rami of C5 and C6. Two nerves arise from the superior trunk which are the subclavian nerve and the suprascapular nerve.
The Middle Trunk: The second trunk or the middle trunk originates directly from the anterior ramus of C7.
The Inferior Trunk: is composed of two nerves via the anterior rami of C8 and T1.
Each trunk then divides into anterior and posterior divisions which pass beneath the clavicle where there are no nerve branches at this level as can be seen from my painting in figure 1 where the dotted golden lines represent the divisions that pass beneath the clavicle (4).
The Divisions
Overall, there are six divisions comprising of an anterior and posterior division from each of the three trunks with three anterior division fibres supplying flexor muscles and ultimately give rise to nerves associated with the anterior compartments of the upper limb (3). The posterior division fibres tend to supply extensor muscles and give rise to nerves associated with the posterior compartments of the upper limb (3).
The Cords
The cords are the fourth section of the brachial plexus, are named based on their positioning with respect to the axillary artery found distally to the clavicle and at this level are termed 'the infraclavicular brachial plexus ' (5) (Figure 6). The cords, axillary artery and vein are located deep to the pectoralis minor and major muscles in the infraclavicular fossa and is a target site for anaesthesia of the upper limb and for brachial plexus nerve blocks.
The cords are formed as follows:
The Lateral Cord (on top):
The lateral cord gives gives a branch to the lateral root (or 'head') of the median nerve and gives rise to the lateral pectoral nerve before it continues into the upper limb as the musculocutaneous nerve (figure 1 and 2).
The distal branch of the lateral cord, the lateral pectoral nerve, innervates the clavicular head of the pectoralis major and weakness indicates lateral cord injury (4).
The Posterior Cord (in the middle):
The posterior divisions of all three trunks unite to form the posterior cord which means that they receive input from all levels of the brachial plexus (C5 to TI). The posterior cord gives rise to three branches before it terminates as the axillary nerve and the radial nerve; namely, the upper subscapular nerve, the thoracodorsal nerve and the lower subscapular nerve.
The Medial Cord (at the bottom):
The medial cord is the continuation of the anterior division of the inferior trunk, and like the posterior cord, it gives off three branches before it terminates as the ulnar nerve. These branches are the medial pectoral nerve, the cutaneous nerve of the arm, and the cutaneous nerve of the forearm (figure 1 and 2).
Injuries:
Medial Cord Injury:
The union of the two anterior divisions of the superior (or upper) and middle trunks form the medial cord. The medial cord gives a branch; the medial root of the median nerve and continues as the ulnar nerve (Figure 2) (3).
Injury to Medial and Lateral Cords and How it May Affect the Pectoralis Major Muscle:
The medial pectoral nerve that arises from the medial cord and with the branches from the lateral pectoral nerve from the lateral cord innervate the sternocostal head of the pectoralis major muscle (4). Examination of the pectoral major muscle is necessary to localize a cord level injury as pectoralis major clavicular head (which creates humeral flexion) involvement implies lateral pectoral nerve injury and sternocostal head (which adducts the humerus) involvement of the pectoralis major implies injury to both the lateral and medial pectoralis nerves, i.e. both medial and lateral cords (4).
Erb-Duchenne Palsy - Upper Brachial Plexus Injury
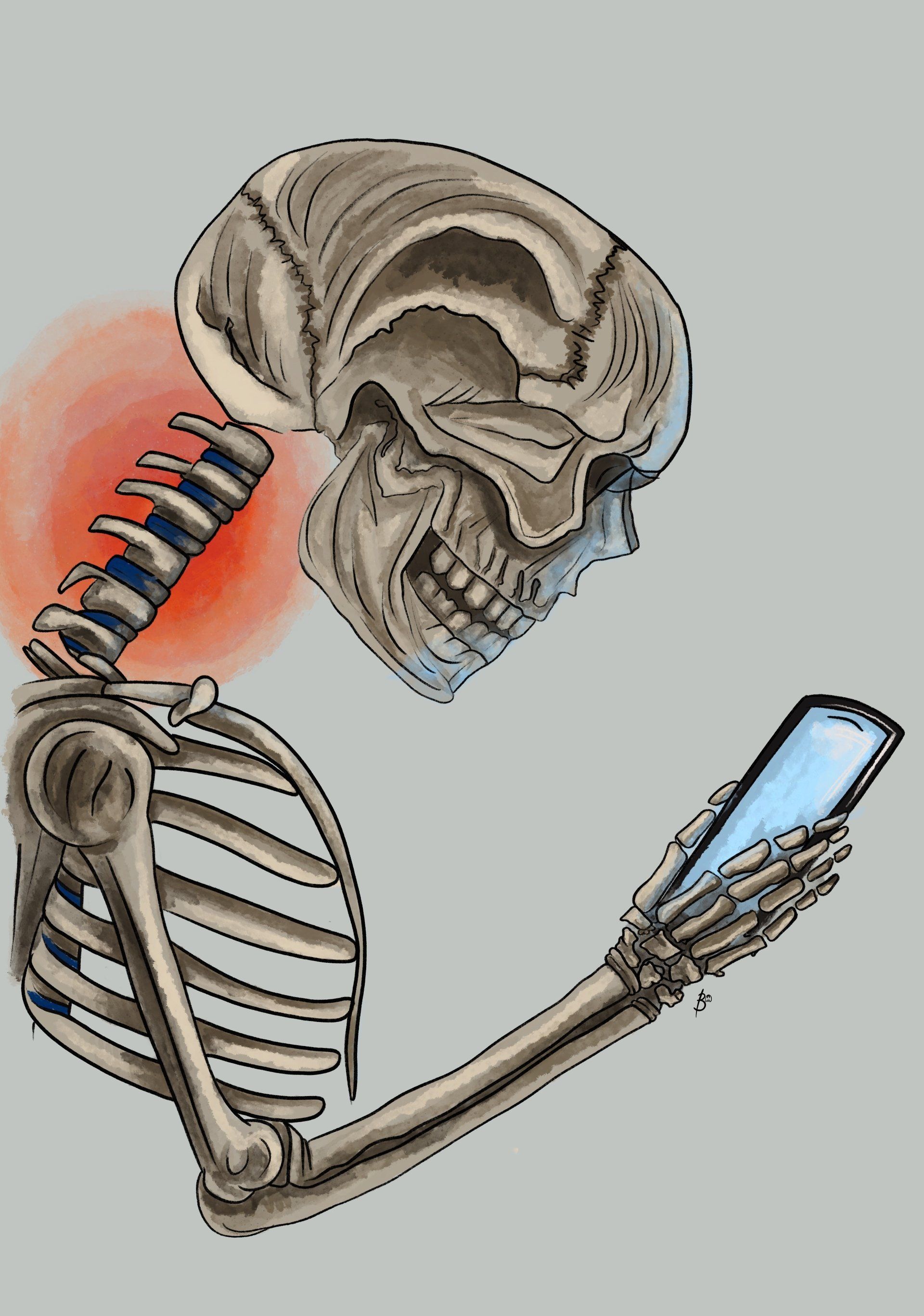
Also known as 'waiter's tip deformity' and named after the neurologists Wilhelm Erb and Duchenne de Boulogne who first described this condition which commonly occurs during an excessive increased angle between the neck and shoulder. Anatomically, the cephalic portion of the brachial plexus C5, C6 and occasionally C7 is either stretched and or at worse torn which can happen during child birth or shoulder trauma (e.g. motor bike accidents or sports e.g. during rugby scrums) (10).
Typically, the presentation of an affected limb is to hang limply and be held in adduction with internal rotation at the shoulder jointfrom the unopposed action of the pectoralis major muscle (10). At the elbow joint, there is extension and pronation caused by atrophic muscle changes within biceps brachii and spasticity of the wrist flexors along with flexion of the fingers (10). This overall presentation has contributed towards the term "waiter's tip deformity". The typical symptom is numbness (anaesthesia) along the lateral aspect of the arm.
The most commonly involved nerves include suprascapular nerve, musculocutaneous nerve, axillary nerve and nerve to subclavius. The muscles which are affected include deltoid, supraspinatus, teres minor, subclavius, infraspinatus, biceps, supinator, coracobrachialis, and brachioradialis muscles of the upper limb (10).
In a neonate post birth, the neurological examination is characterized by the absence of Moro’s, biceps, and triceps reflexes of the affected upper limb with the presence of grasp reflexes as interossei muscles are not affected (8). Sometimes diaphragmatic paralysis is also seen if associated paralysis involves C3 and C4. At this age, treatment involves conservative management with performing physiotherapy and exercises to prevent muscle contracture which starts 7-10 days post injury and overall has excellent prognosis with good neurological outcome (8).
Klumpke's Palsy: Lower Brachial Plexus Injury
Named after the French neurologist; Augusta Dejerine-Klumpke, Klumpke's palsy is a neuropathy and rare form of paralysis involving the muscles of the forearm and hand. It is the result from a lower brachial plexus injury in which the eighth cervical (C8) and first thoracic (T1) nerves are affected. Interestingly, Merryman and Varacallo (2018) have found that approximately 50% of all brachial plexus injuries happen between the age of 19 to 34 (2).
The injury is usually caused via traction on an abducted arm in circumstances from e.g. a neonate being pulled from the birth canal by an extended arm above the head or with someone catching themselves by a branch as they fall from a tree (11).Another cause could be from a compression injury and cause similar signs and symptoms via an apex lung tumor which may press on the cervical sympathetic ganglia of C8 to T1 nerve roots and sympathetic involvement can cause a Horner's syndrome presentation (7).
The classic presentation of Klumpke's palsy is the “claw hand”, as all the intrinsic muscles of the hand are affected with a supinated forearm, the wrist becomes extended with the fingers flexed. If Horner syndrome is present, there is miosis (constriction of the pupils) in the affected eye (11). Thus, the ulnar and medain nerves are affected and a loss of sensation along the medial side of the arm is usually reported (10).
For an open related injury i.e. there is an open fracture,obvious break through the skinor severe vascular compromise, emergency surgery in this instance would required. For closed injuries, conservative treatment via physiotherapy may includes strengthening and stretching exercises the supportive and affected surrounding muscles to help maintain the range of motion and aid a full recovery (7).
If there is no improvement post 3 to 6 months of injury, surgery would be a requirement which would involve nerve grafting. In cases of injuries proximal to the dorsal root ganglion, neurotization or nerve transfer is most recommended which can be defined as 'the transfer of a healthy but less valuable nerve or its proximal stump reinnervating a more important sensory or motor territory that has lost its innervation through irreparable damage to its nerve' (6). Merryman and Varacallo (2018) note that in most cases, the nerves will eventually heal and spontaneous recovery from nerve palsy is possible, but most C8-T1 nerve palsies do not recover without intervention.
How Might Osteopathic Treatment Help?
After performing a clinical assessment, osteopathic manual therapy treatment techniques might be applied to the muscles and joints of the upper ribs, neck and mid back. Home exercise advise might be given to improve related muscular strength and posture control.
References
1. Dictionary.com, https://www.dictionary.com/browse/brachial
, [online] last viewed 11/10/2020
2. Kattan, A. E., Gregory H. Borschel, G. H. (2011) Anatomy of the Brachial Plexus,
Journal of Pediatric Rehabilitation Medicine: An Interdisciplinary Approach
; 4: 107-111.
3. Kenhub (2020) https://www.kenhub.com/en/study/the-brachial-plexus
[online] last viewed 18/10/2020.
4. Kim, D. H., Murovic, J. A., Kline, D. G. (2004) Brachial Plexus Injury : Mechanisms, Surgical
Treatment and Outcomes,
https://www.jkns.or.kr/upload/pdf/0042004153.pdf
[online]last viewed 11/10/2020.
5. D’amore, A., Conte, G., Viglianesi, A., Chiaramonte, R., PERO, G. Chiaramonte. (2010)Evaluation of a Patient with Klumpke’s Palsy
A Case Report,The Neuroradiology Journal; 23: 325-328.
6. Narakas, A. O., Hentz, V. R. (1988) Neurotization in Brachial Plexus Injuries
Indication and Results, Clinical Orthopaedics and Related Research; 237: 43-56.
7. Merryman, J., Varacallo, M. (2018) Klumpke
Palsy,
StatPearls, NCBI Bookshelf: 1-4.
8. Patil, D. Y. (2016) Duchenne-Erb’s palsy in newborn: Result
of birth trauma,Medical Journal of Dr. D.Y. Patil University, 9; 2: 274-276.
9. Snell, R. S. (2007) Clinical Anatomy By Systems, Lippincott Williams & Wilkins.
10. Teach Me Anatomy; The Brachial Plexus, plexushttps://teachmeanatomy.info/upper-limb/nerves/brachial-plexus/
[Online]
Last visited 13/10/2020.
11. Wikipedia, Klumpke Paralysis, https://en.wikipedia.org/wiki/Klumpke_paralysis
, [online]last viewed 18/10/2020.